Fungal Skin
What is a fungal infection?
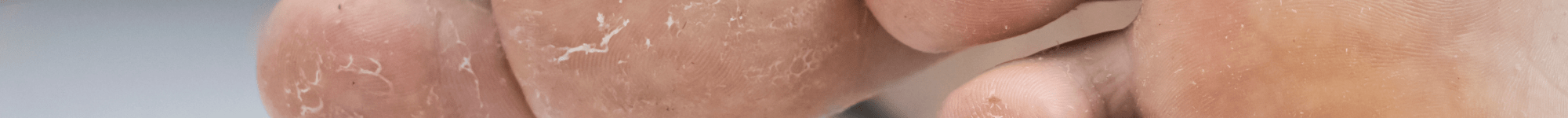
Fungal skin is infected by fungi, a type of pathogen that exist in many forms (microscopic particles to large mushrooms). They are everywhere and don’t usually cause any problems. However occasionally they can settle down and grow in places where they shouldn’t i.e. on our bodies like our skin, nails, between our toes.
What causes fungal skin?
The dermatophytes infect the keratinized tissue of the epidermis – the body’s outer skin layer.
Tinea pedis is a foot infection due to a dermatophyte fungus. It is the most common dermatophyte infection and is particularly prevalent in hot, tropical and urban environments.
- Interdigital involvement is most commonly seen (this presentation is also known as athlete’s foot, although some people use the term for any kind of tinea pedis).
- Tinea pedis may be accompanied by groin (tinea cruris), hands (tinea manuum) and nails (tinea unguium).
The three most common dermatophyte fungi causing tinea pedis are:
- Trichophyton (T.) rubrum
- T. interdigitale, previously called T. mentagrophytes var. interdigitale
- Epidermophyton floccosum
Who does it affect?
It can infect anyone including the younger population and affects up to 59% adults. Source: ( British Association of Dermatologists, BAD)
Dermatophytes requires a small breach in the epidermis commonly caused by either hyperhidrosis or hypohisdrosis. Common transmission routes are using a shared towel, or walking barefoot in a public changing room.
Other risk factors include:
- Occlusive footwear (for example, heavy industrial boots)
- Excessive sweating (hyperhidrosis)
- Underlying immunodeficiency or diabetes mellitus
- Systemic corticosteroids or immune suppressive medications
- Poor peripheral circulation or lymphoedema.
What can help fungal skin
- meticulous drying of feet (especially inbetween and back of toes)
- avoidance of occlusive footwear
- use of barrier protection (sandals) in communal facilities
What are the treatment options
- Topical antifungals
- Oral antifungals
What happens if left untreated?
If treatment of tinea pedis is unsuccessful or untreated the skin may become further broken down causing maceration or even allowing entry of bacterial infection. Reoccurring infection may lead to a coexistent untreated fungal nail infection.
How do we prevent recurrence of fungal skin infection?
To minimise recurrence of tinea pedis:
- Dry feet and toes meticulously after bathing
- Use desiccating foot powder once or twice daily
- Avoid wearing occlusive footwear for long periods
- Thoroughly dry shoes and boots
- Clean the shower and bathroom floors using a product containing bleach
- Treat shoes with antifungal powder/spray i.e. Lamisil spray

