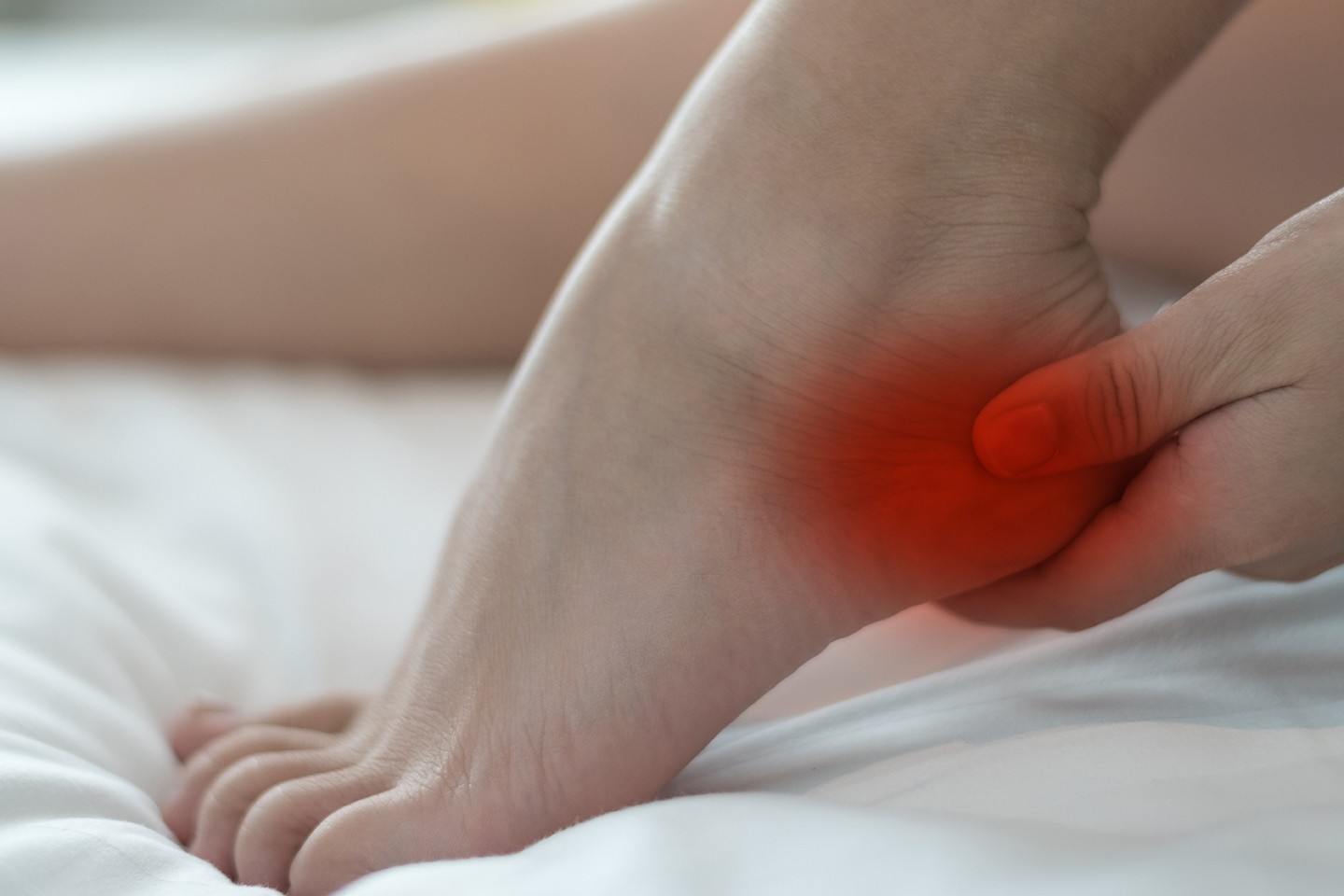
What is heel pain?
Are you or someone you know suffering with heel pain? Scared to take that first step in the morning or has it stopped you from enjoying walking and sports. If you have heel pain you are in the company of many people who have foot pain, accounting for many visits to healthcare professionals – including […]